Research











The Wenzel Lab is focused on the role of biomechanical force generated by flow of fluids such as blood and lymph in determination of cellular fate, motility behaviors, and modulation of the immune system. Specifically, we have identified three key, previously unrecognized roles of mechanotransduction which could be leveraged for novel treatments in patients with hematological disorders, immune dysfunction, and cancers:
1. Vascular force regulates fate decisions and energy metabolism during hematopoietic stem cell specification and expansion.
2. Immune modulatory function of mesenchymal stem cells is stimulated by fluid shear stress with implications for regenerative therapies and the tumor microenvironment.
3. Metastatic programs can be initiated by force associated with lymphatic flow and the tumor microenvironment via YAP1/TAZ.
Our research is designed to address basic biological questions, yet the clinical relevance of our findings has made this work competitive for funding from the NIH, private foundations, and industry partners.
A major obstacle to success of hematopoietic stem cell (HSC) transplantation in treatment of blood disorders and hematologic cancers continues to be the limited supply of compatible, high-quality donor stem cells. This difficulty has motivated global improvements in donor recruitment and matching, as well as aggressive pursuit of new strategies for development of patient-derived or universally compatible hematopoietic cells. Partial success in derivation of HSCs from alternative sources such as pluripotent stem cells has relied heavily on modeling developmental cues in the embryo. Yet, recapitulating in a culture dish the dynamics and complexity of hematopoietic development in vivo remains a significant impediment to generation of scalable HSCs in vitro for clinical use and blood disease modeling (Differentiation 2013).
In the embryo, HSCs are specified from unique endothelial cells that line the arterial vasculature, termed hemogenic endothelium. We have shown that blood flow is required for differentiation of hemogenic endothelium and HSCs (Nature 2009, J Exp Med 2015), and this was confirmed in parallel studies by our collaborators. Indeed, we found that defective hematopoiesis in mutant embryos that lack a heartbeat can be rescued by ex vivo application of fluid shear stress modeled after intensities within the murine aorta (5 dyne/cm2). Flow triggers signaling critical for hematopoiesis, including nitric oxide and prostaglandin E2 (PGE2)-PKA-CREB, which can be mimicked pharmacologically to enhance hematopoietic activity from pluripotent stem cells and cells from the para-aortic splanchnopleura (PSp) / aorta-gonad-mesonephros (AGM), an evolutionarily conserved “hotspot” of HSC fate specification.
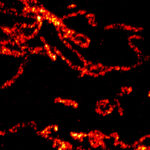
Our data shows that shear stress also stimulates changes in metabolism and mitochondria, including amplification of mitochondrial capacity, transmembrane potential, oxidative phosphorylation, and cristae complexity. We identified a role for the mitochondrial permeability transition pore in regulation of mitochondrial inner membrane maturation that is important for HSC repopulating potential (Commun Biol 2024). Metabolic features of adult HSCs have been linked to hematopoietic reconstitution potential and fate selection. Mitochondrial turnover, activity, and fuel usage play key roles in self-renewal, lineage potential, autophagy, DNA damage, and aging in the adult HSC. Since mitochondria are essential regulators of stem cell fitness that could be manipulated to improve hematopoietic stem and progenitor cell potency and expansion, we are interrogating how shear stress contributes to mitochondrial regulation during HSC specification.
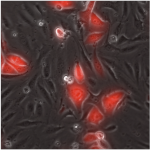
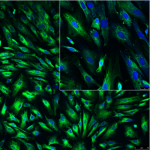
Mesenchymal stem/stromal cells (MSCs) have attracted great attention for their roles in maintaining homeostasis of the hematopoietic system, contribution to the tumor microenvironment, and as regenerative therapeutics for an array of diseases and injuries. Physical forces have been shown to direct differentiation and maturation of MSCs in tissue engineering applications; however, the effect of fluid force on immunomodulatory and related trophic activity of MSCs has been largely overlooked. Recently, we showed that biomechanical cues contribute uniquely to the genetic signaling that dictates MSC immunomodulatory and reparative activities (Diaz et al. and Kota et al. Stem Cells 2017, Cellular Signalling 2017). Transient exposure of human MSCs to fluid shear stress typical of frictional forces present on the luminal lining of human arteries (15 dyne/cm2) stimulates production of anti-inflammatory and anti-oxidant mediators PGE2, HO-1, and IL-1Ra. Transcriptome analysis shows activation of TGFB1, PDGF BB, and HGF signaling, factors critical for MSC engraftment and regenerative activity in organs such as the brain, lungs, and intestine. The topmost physiological systems predicted to be impacted are tissue development, hematological system development and function, and hematopoiesis.
We have shown that several classic mechanotransduction pathways and second messengers are stimulated by shear stress (Cellular Signalling 2017), including calcium ion flux and activation of Akt, MAPK, and focal adhesion kinase (FAK). Preconditioning by transient exposure to shear stress stimulates MSC anti-inflammatory activity to potently suppress production of the cytotoxic proinflammatory cytokine TNF-alpha by activated M1-type macrophages, CD4+ T cells, and NK cells in MSC-immune cell coculture. Approximately three times as many static-cultured MSCs are required to suppress TNF-alpha to a level equivalent to shear-exposed MSCs. This elevated potency depends upon the ability of FAK to stimulate COX2 induction, as chemical inhibition of FAK, but not PI3K-Akt or calcium signaling, reduces MSC efficacy. This enhanced anti-inflammatory activity of MSCs has translational applications. In fact, we showed in a preclinical animal model of neurotrauma that delivery of shear-conditioned MSCs reduces microglial reactivity in injured inflamed brain better than standard, static cultures of MSCs (Stem Cells 2017). This work highlights that shear stress potently and durably alters the milieu of immune regulatory factors produced by MSCs.
Mechanical features of the tumor microenvironment are altered by changes in tissue architecture and density, cellular composition, extracellular matrix deposition, immune cell infiltration, presence of microvasculature, and interstitial fluid flow and pressure. Metastasis is a major determinant of prognosis and the leading cause of mortality (>90%) in cancer patients. Most metastatic carcinomas initially spread from the primary tumor through the lymphatic system, a vascular network that drains interstitial tissue fluid into regional lymph node basins. This egress route exposes cells to fluid frictional force associated with flow of fluid from surrounding tissues.
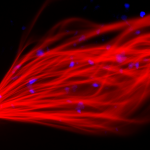
We have shown that shear stress typical of flow within initial lymphatics (<0.2-1 dyne/cm2) induces expression of a network of genes in prostate cancer cells with roles in cell migration, proliferation, and survival (Nature Communications 2017). Indeed, we find that shear stress enhances cancer cell motility and entry into the cell cycle through two transcriptional coactivators recently recognized for their sensitivity to mechanical cues – YAP1 and TAZ. YAP1 and TAZ lie downstream of the Hippo tumor suppressor pathway, which regulates their localization to the nucleus via post-translational modifications that limit access to DNA and thus transcriptional activity. Regulation of YAP1/TAZ is also thought to occur independently of Hippo signaling, especially in the context of mechanotransduction, but relies on similar means of post-translational regulation and cytoplasmic sequestration to dictate access to the nucleus. Importantly, flow-induced cell motility in prostate cancer strictly depends upon YAP1 activation, as inhibition of YAP1 or the YAP1-TEAD transcriptional complex by genetic, pharmacological, or small interfering peptide approaches blocks taxis. Despite the high homology and overlapping functions of YAP1 and TAZ, inhibition of TAZ has no effect on cell migration. Instead, TAZ activity induces transcription of a subset of YAP1/TAZ target genes independently of YAP1 to drive increased DNA synthesis and cell cycling (Cell Cycle 2018). This increased proliferation can be abrogated by genetic disruption of TAZ. This recent body of work suggests that YAP1 and TAZ play distinct roles in the response to mechanical cues and identifies the YAP1-TAZ signaling axis as a central component of the mechanosensory machinery that promotes flow-induced motility and proliferation of cancer cells.
Our data support emerging evidence for the critical role that mechanical stimuli in the tumor microenvironment play in cancer progression, and we believe that these approaches could broaden therapeutic options for high-risk cancers by targeting of tumor-specific mechanotransduction pathways to block cancer cell motility and anoikis resistance in the lymphatics. A number of intriguing questions remain, especially regarding how fluid force is transmitted into an intracellular signal to regulate YAP1/TAZ. This regulation likely occurs via post-translational modification and interaction with binding partners, but our work has only partially elucidated the upstream signaling which involves Rho kinase, the actin cytoskeleton, cofilin, and LIM kinase. Indeed, our study of breast cancer cell motility highlights critical differences in response to flow that are dictated by RhoA GTPase activity which appears to override the regulatory effects of YAP1 (FASEB BioAdvances 2022). Additionally, few groups have described differences between YAP1 and TAZ in terms of function and transcriptional targets. These aspects of YAP1/TAZ mechanotransduction represent high priority areas of investigation if we are to identify druggable targets to block the activity of these transcriptional cofactors.